Green healthcare facilities
Courtesy : www.managedhealthcareexecutive.com
From Recycling and waste management programs to nontoxic paint and permeable pavement, hospitals across the country are implementing green initiatives to produce healthier environments for patients and staff, which they say saves not only energy, but money.
Among several provider facilities going green is Stony Brook University Hospital, in Stony Book, N.Y., which recently signed an agreement with the U.S. Environmental Protection Agency (EPA). The agreement outlines energy and water conservation, waste management and the use of environmentally friendly products, and the hospital is currently auditing areas to reduce energy consumption.
“A hospital is unique in that it’s a structure that operates 24/7,” says Andrew Bellina, EPA program coordinator, “So, there are opportunities for powering down in many areas of the hospital that do not impact the people that are working or the care of the patients.”
In addition, the hospital is taking on a number of initiatives designed to reuse materials and reduce material waste. For example, staff has eliminated the blue, disposable wrapping used for sanitary operating tools, says Bellina. Tools now arrive in reusable containers.
However, he notes, the hospital has to evaluate recycling from a practical standpoint while also maintaining strict accreditation standards. Even so, recycling at the hospital increased by about 420 tons in 2007 and 2008, and it is expected to be higher this year.
“It significantly affects your carbon footprint when you recycle waste instead of just throwing it out, because you don’t go through the actual mining, the treatment, the procurement, the manufacturing and the transportation,” he says. “You’re cutting all that out.”
Water conservation is another important aspect of the agreement struck with the EPA. Bellina notes water supply costs recently increased 20% in New York City. He predicts water shortages in as many as 36 states in the next three to five years.
The hospital is looking to conserve water in two ways. First, captured storm water can be reused for non-contact functions, such as watering lawns and landscaping. Second, he says, it will be important to reduce demand for water. The hospital is monitoring water use with equipment that limits water flow and reduces total use.
Going green will definitely show a return on investment in the long run, and in most cases, produce immediate savings, Bellina says.
“Five years ago it [going green] would have cost you money, and the payback would be seven, 10 or 12 years, but now there are immediate cost savings. For example, recycling is an immediate cost saver,” he says, “And you reap the economic benefits through the lifetime of the structure after that.”
Determining effects on the quality of care is not as easy, he says, but he postulates that once the hospital’s energy audits are complete and the air handling is upgraded to a more efficient mix of outdoor and indoor air, the quality of air will improve within the hospital. Better air means better health, especially for those who need respiratory care.
EAST CAROLINA HEART INSTITUTE

The structure has only been open for a year, but was built with energy efficiency in mind, according to Brian Floyd, executive director of the Heart Institute. It also contains recycled materials in the carpet as well as in bathroom, kitchen and ceiling tile.
Natural lighting is one feature that overlaps in the green movement and healthy hospital movement. An effort was made to light the Institute with large windows in patient rooms, physician work areas, waiting rooms, lobbies and cafes.
“Many studies show that people recover faster when they have access to sunlight, and we want to make people as comfortable as possible and acclimate them to the day and night cycles so they can heal faster,” Floyd says.
It also requires less energy to light the facility during the day. With the help of sensors, artificial lighting turns on only when someone is in the room and dims when natural light levels are adequate.
The utility plant powering the Institute operates on energy efficient air conditioning chillers, high-efficiency electric motors and variable-speed pumping and air flow systems, according to Floyd.
The monthly electricity expenses at the Heart Institute have averaged 30 cents per square foot, or $142,000 per month, since opening in January 2009, according to James Ryals, Media Specialist for the Heart Institute and Pitt County Memorial Hospital. To compare, over the same period, monthly electricity expenses in the main hospital have averaged 45 cents per square foot, or $533,000 per month. The main hospital was built in 1977, and is twice as big as the Heart Institute, says Ryals.
“The per-square-foot figures are a better basis for comparison than the monthly totals,” he says. “It’s safe to say that, with the efficiency measures we’ve taken, our power expenses at the Heart Institute are roughly 33% lower than the main hospital.”
Certain intangible cost savings, such as worker productivity, are harder to define, says Floyd, but he has noticed that retention of staff is higher and length of patient stays are shorter.
In Digital Health Space, Many Companies Sidestep Rigorous Study
July 14, 2022
The report highlights the gap between rigorously tested prescription digital therapeutics and products that make health or economic claims without providing supportive evidence.
Even as digital therapeutics have emerged as an increasingly important therapeutic category, a new report shows many digital health companies have avoided rigorous clinical evaluation of their products.
The study, published in the Journal of Medical Internet Research, highlights the gap that often exists between the claims made by digital health software developers and the scientific evidence available to validate their claims.
Simon C. Mathews, MD, of the Johns Hopkins University School of Medicine, was the study’s senior and corresponding author. He and colleagues noted that previous research into the evidence behind digital health tools has often been narrowly focused on a single therapeutic area, or has been limited in scope. In the new study, they wanted to use a wide lens.
“While some of my prior work and other studies have highlighted deficits in digital health, this was among the largest studies to show the real gap between reality and expectations of digital health,” Mathews told Managed Healthcare Executive.
The investigators pulled data from the Rock Health Digital Health Venture Database, the Food and Drug Administration (FDA), and the National Library of Medicine. They searched for companies selling digital health products aimed at prevention, diagnosis, or treatment of medical conditions. In the end, they identified 224 digital health companies, which had been in existence for an average of 7.7 years.
Mathews and colleagues then assigned each company a “clinical robustness” score, based on the number of regulatory filings and clinical trials it had completed. On average, the companies had a score of 2.5, with an average of 1.8 clinical trials per company and 0.8 regulatory filings per company.
However, that average conceals a significant dichotomy: 20% of companies had clinical robustness scores of 5 or greater, while nearly half of companies—44%—had clinical robustness scores of 0.
Mathews said the latter figure is a significant problem for digital health companies.
“For digital health to be taken seriously and seen as legitimate clinical tools, far more companies need to be engaging in the rigorous processes that are required to show efficacy,” he said.
Though many companies had scarce clinical evidence, that did not stop them from making public claims about their product’s efficacy, economic impact, or engagement capabilities. The study found no correlation between the number of public claims a company made and their clinical robustness score, suggesting that many companies made claims they could not back up with rigorous clinical trials or regulatory filings.
In some ways, the study highlights an emerging split between digital health and wellness apps, which are marketed widely and widely available, and prescription digital therapeutics, which are more rigorously tested, require a physician’s prescription, and have been authorized or cleared by the FDA.
Mathews said clinicians should be aware of such differences when they counsel patients about the use of digital health software.
“There are many [digital health products] that provide education and social support that can be helpful and don’t require extra diligence,” he said. “However, for any tools that make any clinical claims, I would have a healthy dose of skepticism. In these scenarios, I would encourage clinicians to review the evidence first to help manage patient expectations.”
Mathews and colleagues said patients will benefit from greater testing and validation of digital health products, but he said the companies also stand to gain by enhancing their legitimacy. Only by more rigorously publishing evidence to back their claims can digital health solutions meet their potential, he said.
“If you are like me and believe they have the potential to deliver more patient-centric care, then you should also expect evidence comparable to traditional clinical treatment options,” he said.
Reference:
Day S, Shah V, Kaganoff S, Powelson S, Mathews SC. Assessing the Clinical Robustness of Digital Health Startups: Cross-sectional Observational Analysis. J Med Internet Res. 2022;24(6):e37677. Published 2022 Jun 20. doi:10.2196/37677
Digital Therapeutic for Substance Use Disorder Drives Down Care Utilization, Cost
July 12, 2022
Patients using the prescription digital therapeutic saw a decrease of $3,591 in healthcare costs in the six months following treatment initiation.
Digital therapeutics firm Pear Therapeutics has released new data showing its prescription substance use disorder (SUD) therapy reduces hospitalizations and lowers healthcare costs for patients.
The data will be published in the journal Advances in Therapy, but the findings are currently available online as a pre-print.
The treatment is called reSET. The app is built around cognitive behavioral therapy (CBT) utilizing the community reinforcement approach (CRA), the company said. It includes a 12-week course of therapy, in which patients are incentivized for completing lessons and abstaining from drug use. The app also includes fluency training designed to reinforce the lesson content.
Previous studies have shown the therapy can be effective at improving rates of abstinence and treatment retention when coupled with usual treatments. In the new report, investigators wanted to know how such improvements might translate into changes in healthcare resource utilization and costs.
The investigators used claims data to identify 101 patients with SUD who had been prescribed reSET. The authors then evaluated healthcare utilization and costs for the patients in the six months prior to the start of reSET treatment and in the six months after starting the therapy. Most of the patients (54.5%) were on Medicaid insurance.
Overall, the data showed a 50% drop in hospitalizations among the cohorts once they started using reSET (incidence rate ratio [IRR]: 0.50; 95% confidence interval [CI]: 0.37-0.67; P<0.001). That included drops in inpatient stays, partial hospitalizations, and emergency department (ED) visits, the investigators said. Patients using reSET also had lower laboratory and pathology costs, the analysis showed.
All of that translated to an estimated $3,591 per patient reduction in healthcare costs in the six months following reSET initiation compared to the six months before beginning the therapy.
“Pear now has a continuum of evidence supporting our 3 FDA-approved prescription digital therapeutics, including randomized controlled trials, real-world clinical data, and real-world health economic data,” said Yuri Maricich, MD, Pear’s chief medical officer and head of development, in a press release.
Maricich said the data were also important because they make a case that prescription digital therapeutics can add value, even if they come at an additional cost to traditional therapeutic approaches.
Pear’s Neel Shah, BPharm, PhD, the study’s corresponding author, noted along with colleagues that the timing was also significant given that the study period of January 2018 to February 2021 included the COVID-19 pandemic era.
“Although hospitalization rates for certain disease states declined during the pandemic (e.g., acute cardiovascular disease and stroke/transient ischemic attack) several published datasets and analyses show that among patients with existing SUDs the rate of ED visits and hospitalizations increased during the pandemic,” the authors wrote.
Previous reports have suggested people with SUDs were more likely to be hospitalized with COVID-19 compared to people without a diagnosed SUD.
Shah and colleagues said their data set is subject to limitations. Costs were estimated based on published literature, and therefore might vary from actual costs. In addition, the data set did not allow for mortality analysis, so they said it is possible some patients might have died during the six-month period after initiating reSET.
Still, Shah and colleagues said the data suggest CBT administered through the reSET program may be an important treatment addition for many patients with SUD.
“The observed per-patient cost reduction of $3,591 in the pre-post analysis suggests that treating patients with reSET may lower overall costs of care, which may be relevant to payors at all levels of the healthcare system,” they concluded.
Hospitals see lower readmissions with more post-discharge options
July 5, 2022
Health systems with more primary care doctors and palliative care services saw fewer people coming back to the hospital, a new study finds.
Hospitals providing a variety of post-discharge care options typically enjoyed more success in helping patients avoid readmission, a new study finds.
Researchers found that hospitals with a larger supply of primary care physicians and health systems that offered palliative care services had lower 30-day readmission rates. Health systems operating in areas with more skilled nursing facility beds or licensed nursing home beds also saw fewer people return to the hospital within 30 days. The study was published Tuesday, July 5 in Health Affairs.
However, the study also found hospitals in areas with a larger number of home health agencies or nurse practitioners saw a higher level of 30-day readmissions.
- Related content: Better transitional care can reduce hospital readmissions
The authors noted that hospitals may want to consider providing additional post-discharge care options to serve their patients and to avoid the prospect of penalties from the federal government. The Centers for Medicare and Medicaid Services reduces payments to healthcare systems if they persistently have higher rates of readmissions.
“Our results suggest that hospitals may take a more active role in the development of postdischarge care options in their communities or partner with existing infrastructure to improve continuity of care and clinical outcomes and to avoid penalties,” the authors wrote.
The authors also suggested hospitals should employ palliative care services where possible.
“Palliative care use may reduce unwanted, potentially unnecessary medical care for seriously ill people, whereas patients in areas without sufficient access to primary care or nursing facilities (for example, isolated rural or low-income urban areas) may be forced to return to hospital emergency departments if complications arise,” the researchers wrote.
Building community partnerships
Researchers examined more than 3,000 hospitals between 2013 and 2019.
Most of the hospitals were private, nonprofit providers based in urban areas, the authors said. Most operated a hospital-based palliative service. The median hospital in the study had fewer than 200 beds and an average daily census of fewer than 100 patients.
Health systems should look for opportunities to work with other community organizations and agencies to help patients after they leave the hospital.
“Our results suggest that hospitals may benefit from work to improve local access to care or hospital-community partnerships to improve continuity of care after discharge,” the authors wrote.
Hospitals should be taking a close look at readmission rates from various discharge sites to determine if patients are faring better in some settings than others and to see where care can be improved.
With higher readmission rates associated with home health agencies, the authors suggest it could be a reflection of a lack of continuity of care due to the high turnover of workers in those agencies.
While a higher rate of nurse practitioners was also associated with a higher likelihood of readmission to the hospital in this study, the authors noted nurse practitioners have shown success in some interventions in helping patients avoid a return trip to the hospital.
The authors speculated that a higher concentration of nurse practitioners in a region may be a sign that patients in that area have a higher level of sickness or health complications, the authors noted. The tie between nurse practitioners and greater readmission rates could also be a reflection of the dearth of other healthcare resources.
Reconsidering penalties
The authors said the study carries implications on how the federal government should be reimbursing hospitals.
CMS should reevaluate some of the ways it examines health systems to determine if they should be penalized under the Hospital Readmissions Reduction Program, the authors suggest.
“CMS may also consider risk adjustment for postdischarge care supply under the HRRP to avoid penalizing or rewarding hospitals based on the characteristics of the communities they serve instead of the quality of care they provide,” the authors wrote.
If CMS adjusts its risk on the availability of a hospital-based palliative care service, it could punish health systems with such services by reducing their readmission targets, the authors said.
Such a move could also deter health systems from launching palliative care services, the authors wrote.
Researchers from Vanderbilt University Medical Center, Veterans Affairs Boston Healthcare System, Washington University in St. Louis, and Boston University wrote the study.
Three Ways to Alleviate Hospital Staffing Challenges through Technology
June 28, 2022
Technology can help cut back on unnecessary administrative tasks, improve task efficiency and better preserve staff resources.
After nearly three years of the pandemic, it appears that the healthcare industry is finally turning a corner. Hospitalizations are trending down, and overwhelmed ICUs have some breathing room again.

However, for many hospital systems, the pressure has increased in other ways. The convergence of COVID-19 and pre-existing staffing challenges is putting immense burden on hospitals, which are also grappling with a rise in complex patient care and growing burnout among staff. Fatigue is driving away nurses from the bedside at an alarming rate, and more than one-third of nurses indicate they are very likely to quit their roles by the end of 2022. Many organizations face the stark reality of preparing for the impending storm.
While hospitals try innovative methods for recruitment and retention — from increasing compensation to partnering with nursing schools to fill the pipeline — the success of these efforts will be hindered without also re-tooling their approaches to workload and improving the day-to-day practices of case management nursing staff.
Case management in its current form involves inefficient, manual processes that make prioritization of tasks difficult, leading to inconsistent reviews and patient status flip-flopping. Not only is this unproductive for staff, but it can lead to delays for patients who otherwise should have been discharged, further straining tight resources. Effectively determining and administering the appropriate level of care for patients is the key to returning case management and utilization management to their patient-centered focus, removing friction — and frustration — within nurses’ jobs.
Technology has many applications within healthcare, and utilization management is no exception. There are three main ways that technology can help alleviate hospitals’ staffing challenges: solving for unnecessary administrative tasks, improving task efficiency and better preserving staff resources.
The myriad of administrative tasks outside of patient care can consume hours and add unnecessary workload to already strapped staff. From reviewing daily patient charts in the EMR to ongoing evaluation of medical necessity, case management nurses often spend the majority of their day on these behind-the-desk tasks.
But it doesn’t have to be this way. Using artificial intelligence technology to automate repetitive work frees up staff to focus their efforts on more complex tasks that require human intervention.
Instead of going top-to-bottom reviewing patient censuses, predictive AI technology can stratify reviews based on risk, allowing for enhanced management and opportunity capture. By automating ongoing rote administrative tasks, hospital staff can work more efficiently, prioritizing their day on the most pressing activities that utilize their expertise. Nurse care managers can spend more time at the bedside with patients, better evaluating discharge readiness and building a solid care transition plan. Giving nurses more time in front of patients also leads to improved job satisfaction, reducing the likelihood of burnout and attrition.
Refocusing nurse case managers on higher risk patients not only saves utilization review resources but improves patient flow through the hospital system as well. This creates a positive feedback loop where patients are appropriately assigned care, allowing for efficient use of resources to ease hospital system strains that have become all too common over the last few years.
The healthcare system is steadily growing more complex, necessitating the implementation of innovative solutions to streamline where possible. By applying AI and machine learning-fueled technologies to review processes, hospitals can transform the way they leverage analytics, enabling staff to become better nurse care managers, better clinical thinkers, and more patient focused, ultimately leading to improved job satisfaction among nurses with a more seamless system for patients and care delivery personnel alike.
Heather Bassett, M.D., is chief medical officer of XSOLIS.
Patients less likely to return to emergency room if they get a phone call: Study
June 21, 2022
Those who received an automated call were less likely to go back to the hospital, researchers found. Those patients were also more likely to have followed up with a clinician.
Patients who received a phone call two days after discharge from an emergency department were less likely to need a return trip to the hospital, researchers have found.
Researchers from the University of California San Francisco and the University of Colorado examined results from thousands of patients at a large, urban, academically affiliated emergency department. In the study published in Jama Network Open, the rates of revisits to the emergency department were “significantly lower” among those who received an automated telephone call two days after discharge.
Among those who received a call, 7.6% of those patients returned to the emergency department within seven days. Meanwhile, 10.3% of patients who did not get a phone call ended up going back to the emergency department within a week.
The study also found an association with return calls and a reduced risk of a return to the emergency department within 72 hours. Only 4.6% of those who were called ended up returning to the emergency room in 3 days, while 6.2% of the patients who didn’t get a call were back in the emergency department within 72 hours.
Patients who received a call two days after discharge also indicated they were more likely to understand their health issues. They were also more likely to have received their medications and followed up with a healthcare clinician, the study found.
“This study suggests that there is measurable value to automated ED callback programs with a clinician contact option,” the authors wrote.
The researchers pointed out that follow-up phone calls represent one strategy to reduce emergency department admissions, thus improving patient care and reducing costs for hospitals.
“Return visits to the ED are a strain on health systems—with substantially increased costs, patient volumes, treatment delays, and mortality,” the authors wrote. “Reductions in ED revisits represent an opportunity to improve care and have been used as a quality metric for some time.”
Roughly four in 10 patients in the study (40.9%) were Hispanic, while more than one in five were Black (22.1%).
Calls to patients were conducted in English, Spanish, and Cantonese, but the preferred language among most patients (74.9%) was English. The study noted a sizable portion of patients (13%) were either homeless or in “marginal housing.”
Patients who received the calls were given questions with prompts to respond. Patients were asked if they had questions about discharge instructions or follow-up plans for treatment. They were also asked if they had questions about medications that were prescribed or recommended in the emergency department. Then they were asked if they had a different type of question.
Patients responded by using the touch-tone buttons on their phones. Patients didn’t need smartphones to respond to the questions.
Patients who received a two-day call also fared better in some other measures, though the researchers said the gaps weren’t statistically significant.
Those who were called were more likely to have received their medications compared to those who didn’t get a call (87% to 83.6%). The patients who got an automated call were also more likely to understand their health conditions (77.5% to 74.9%) and were more likely to follow up with a clinician than those who did not (67.9% to 66.3%).
The researchers noted that a little over 30% of patients were reached by phone two days after discharge, and 21% were reached again at 14 days.
“Patients with significant social needs, especially those without a reliable telephone or housing, have been shown to use the ED more often and may be missed by this intervention,” the authors wrote.
Scott Fruhan, an emergency medicine physician at the University of California San Francisco and Corey B. Bills, a doctor at the University of Colorado School of Medicine, wrote the study.
ACO Update: The Pathways to Success Program
June 17, 2022
MHE Publication,
The program implemented by the Trump administration is designed to put more Medicare Shared Savings Program ACOs into two-sided risk. An industry group has discouraged participation in the program.
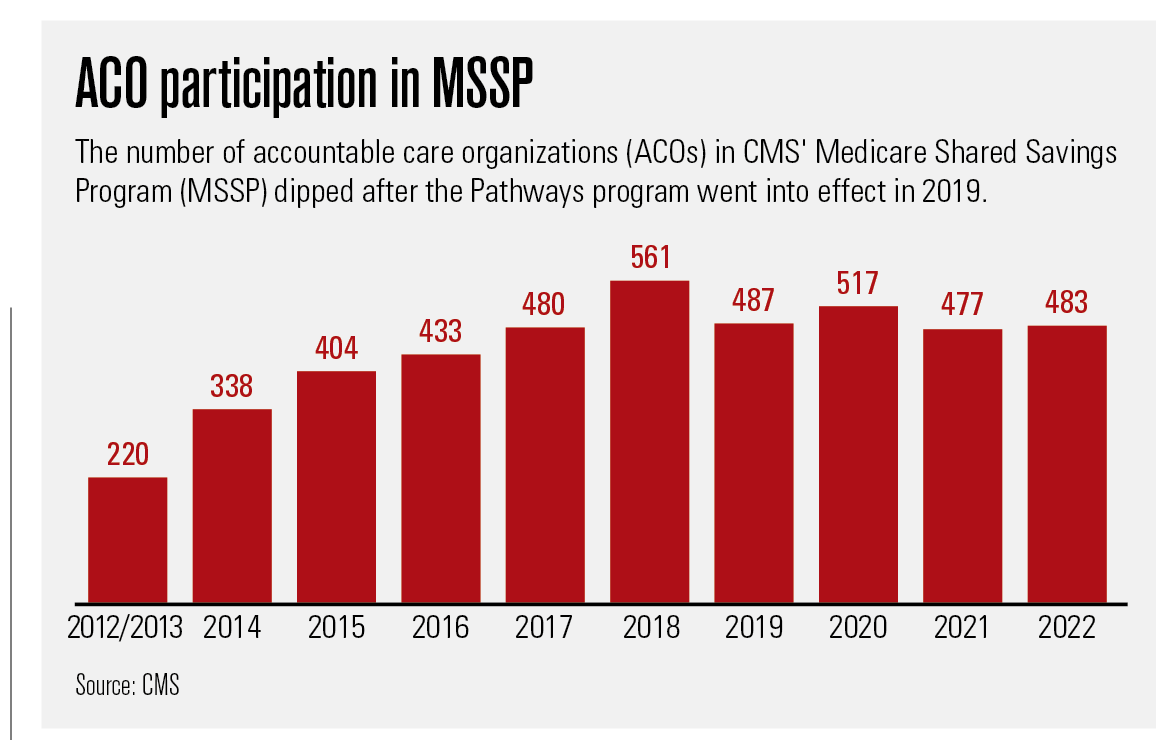
Since its inception in 2012-2013, the CMS Medicare Shared Savings Program (MSSP) has cranked along like a roller coaster climbing steadily upward. Starting with 220 participating accountable care organizations (ACOs) and 3.2 million beneficiaries, it reached the high point in 2018 with 561 organizations covering 10.5 million people.
That was the same year that CMS unveiled Pathways to Success, its overhaul of MSSP’s ACO program aimed at increasing cost savings for the Medicare program by requiring more MSSP ACOs to assume two-sided risk: upside “shared savings” if they come in under budget for their attributed population but also downside “shared losses” if they go over it. The number of participating ACOs fell to 487.
Since then, the MSSP ACO program has oscillated between shallow valleys and modest peaks of ACO participation, growing by 30 organizations in 2020, losing 40 in 2021, and adding 6 this year. The number of beneficiaries covered has, though, held relatively steady with 11 million at the beginning of this year, or about one-third of the 33 million beneficiaries in traditional Medicare.
A number of factors contribute to those numbers, including the normal ebb and flow of ACOs joining and leaving the program and consolidation of providers. The winding down of another CMS ACO program, called Next Generation, had some ACOs looking for a new home.
Then there is what David Muhlestein, Ph.D., J.D., calls the “really big driver”: the COVID-19 pandemic.
“It has made people completely rethink what their priorities are, and anything related to ACOs is just so much less important right now,” says Muhlestein, chief strategy and chief research officer for Leavitt Partners, a healthcare consulting firm in Salt Lake City.
Jennifer Gasperini, director of regulatory and quality affairs for the National Association of ACOs (NAACOS) agrees that the pandemic and all those other issues are at play. But the way she sees it, Pathways is the main reason.
“We definitely think that Pathways has had an effect on the overall interest in the program,” she says. “Pathways decreased the incentive to participate by doing two things: reducing the shared savings that you can keep if you are successful and pushing (ACOs) to risk more quickly.”
Industry observers say it can take an ACO at least three years to get its sea legs. That timeline is about right, Muhlestein says. But CMS, he notes, is looking at a different timeline and issue: saving Medicare, a program under financial stress as it takes on the baby boom: “If you have a bunch of organizations that won’t take downside risk and will only stick around as long as there is a possibility of getting payment, can you say they are really making substantive changes to improve care and lower costs?”
Two-sided risk sooner rather than later
Accelerating assumption of two-sided risk is the most important difference between the Pathways program implemented by the Trump administration and the original MSSP. Pathways sorted the prior MSSP’s multitrack options down to two, Basic and Enhanced, although the Basic Track has five stages. ACOs newly entering the Basic Track have a two-year period of upside-only risk and 40% shared savings. After that, they are on a three-year schedule of two-sided risk that dials up the shared-savings percentages but also creates greater exposure to shared losses.
The Enhanced Track puts ACOs right into two-sided risk with shared savings of 75% and shared losses of between 45% to 75%. But, importantly, the Enhanced Track also qualifies the ACO as an Advanced Alternative Payment Model, which makes it eligible for incentive payments under a different CMS program.
ACOs that were participating in MSSP prior to Pathways could enter the Basic Track at its various stages depending on their revenues, how long they had been participating in MSSP and other factors. According to a CMS report earlier this year, as of Jan. 1, 2022, 337 of the 483 (70%) ACOs in the Pathways version of MSSP were participating in the program’s Basic Track, and 190 (56%) of those were still in the two-year period of one-sided risk. The other 146 jumped right into the Enhanced Track.
Muhlestein is a fan of the Pathways effort to push ACOs into assuming two-sided risk sooner: “I think that making people move toward risk makes it real and requires them to think about things in a way they probably didn’t before,” he says. “I think, basically, it says quit experimenting and start doing, which is a major difference (from) what has happened in the past.”
The Pathways rules also changed some of the benchmarking methods used to set the financial goals of the ACOs and therefore their eligibility for shared savings and losses.
Although NAACOS generally approves of CMS’s benchmarking changes, the group is concerned about what Gasperini dubs the “rural glitch.” For instance, an ACO representing half the care in a smaller region may improve by 5% in a year. That means that, on average, the whole region improved by 2.5%. By exclusively comparing the ACO to its region, the ACO is literally competing against itself.
“This is about the idea of having to constantly kind of beat yourself,” Gasperini says. “That is one issue that we think, if changed, could really go a long way toward sustainability in the program.”
Pathways rules have some benefits for the participating ACOs. They can also permit the bypass some Medicare restrictions on telehealth services. (Because of the COVID-19 Public Health Emergency and its telehealth waivers, the telehealth perk hasn’t meant as much as it might have). Additionally, Pathways waives a Medicare rule that limits coverage of rehabilitation in a skilled nursing facility to beneficiaries who were discharged to the facility after three consecutive days in a hospital. The Pathway rules also allow ACOs to make $20 incentive payments to beneficiaries to take steps such as joining a wellness program that are believed to lower costs and reduce the risk of serious illness.
NAACOS has viewed the declining number of ACOS in MSSP with alarm. When the CMS released the figures earlier this year, NAACOS issued a press release that quoted its chief executive officer, Clif Gaus, Sc.D., M.H.A., as saying they showed a “shrinking of this important ACO model.” According to NAACOS, 18 of 46 new ACOs participating in the program are former Next Generation participants and so not really new ACOs.
Many of NAACOS’ concerns would be remedied if a bipartisan bill stalled in the House were to gain traction. Introduced in July 2021, the Value in Health Care Act of 2021 would bump MSSP’s Basic Track shared-savings rate back to 50% and give ACOs at least three years in the one-sided risk mode.
Meanwhile, NAACOS continues to meet with the Biden administration to discuss adjustments to MSSP ACO, including new incentives and grants that would help attract practices. The administration, Gasperini says, is “engaged with us and, I think, committed to value-based care, and hopes it or CMS, or Congress, will make some changes to Pathways before the end of the year. Now it’s really about putting pen to paper and making some of these changes so that we can see increased participation.”
Like Gasperini and NAACOS, others are also waiting to see which direction the Biden Administration takes with the ACO program.
“The big one is what is the Biden administration plan?” says Muhlestein. “That is really going to influence in the next couple of years how much activity takes place and how active people are. I would fully expect them to come up with a full plan, both from the (CMS) Innovation Center as well as CMS for the MSSP.”
Patients With Cancer Faced Heightened Economic, Social, Psychological Impacts From COVID-19
June 15, 2022
A review of multiple studies found the COVID-19 exacerbated the economic, social and psychological difficulties that patients with cancer were already facing because of their cancer.
Patients with cancer regularly face economic, social and psychological impacts that were compounded by COVID-19. In a new study published in Supportive Care in Cancer, researchers reviewed approaches to minimize the impacts of COVID-19 on patients with cancer.

“Cancer patients were particularly vulnerable to [the pandemic’s] adverse impacts given their reliance on the healthcare system, and their weakened immune systems,” wrote researchers led by Ann Kirby, Ph.D., of the Department of Economics, Cork University Business School, University College Cork in Ireland.
The researchers conducted a systematic review to examine the social, psychological and economic impacts of the pandemic on patients with cancer with the included studies capturing the experience early in the pandemic when severe restrictions were in place worldwide.
The review included 56 studies, 96% of which were single-country studies. Overall, 20% of the studies were from the United States and 27% from Europe (18% from Italy.specifically). The studies mostly included patients with multiple cancer types (64%) followed by 18% focusing on breast cancer.
The social and psychological impacts of COVID-19 on patients with cancer that were reviewed included worry, fear, distress, anxiety, depression, social isolation and loneliness. Among the studies, there was a heightened sense of fear that the cancer would recur or progress because of care delays and disruptions.
Patients were also afraid of getting COVID-19. A study of Italian patients found 37.3% of patients with cancer were very or extremely afraid of going to the hospital and contracting COVID-19 and 24.5% were very or completely afraid that being protected against COVID-19 would be more important than continuing their cancer care.
While some patients were willing to postpone or delay their treatments for cancer, patients mostly prioritized cancer care over the fear of contracting COVID-19. According to the authors, the review found deliberate appointment delays were associated with depression and anxiety about cancer progression, and a delay to posttreatment follow-up or palliative care exasperated these feelings even more.
As a result of stay-at-home orders, quarantines and the fear of infection, a number of studies highlighted social isolation and loneliness experienced by patients with cancer. For instance, young cancer patients between the ages of 18 and 39 years reported feeling more isolated compared with before the pandemic.
“Some patients’ perceived risk of COVID-19 infection caused them to engage in extreme levels of social isolation where they had no visitors and lived alone,” Kirby and her co-authors explained. “For others, the pandemic exasperated underlying situations.”
In addition, the financial burden many patients with cancer feel was exasperated during the pandemic. While patients in the United States saved time and money due to the transition to telemedicine, treatment changes cost patients more in Jordan, the authors found. In countries that required negatives COVID-19 test results to attend appointments, patients were faced with additional costs that influenced decisions to undergo cancer treatments for some patients, particularly those in poorer countries.

A fascinating discussion is definitely worth comment. I think that you ought to write more on this issue, it may not be a taboo matter but typically people dont discuss these topics. To the next! All the best!!